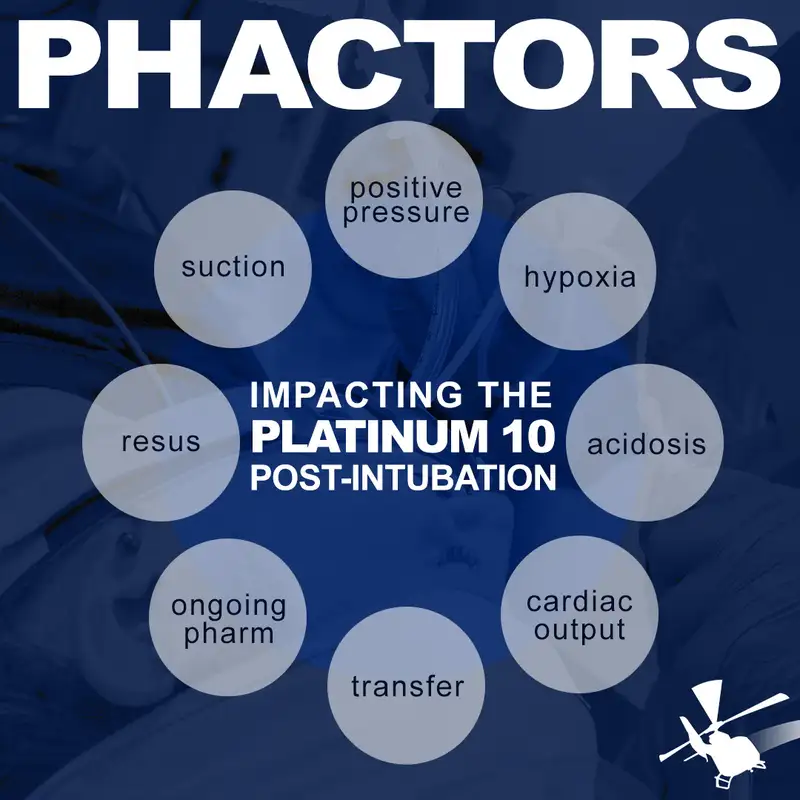
PHACTORS: Impacting the "Platinum 10" Post-Intubation
Download MP3In this engaging and insightful episode of the FlightBridgeED Podcast, Eric Bauer is joined by Dr. Michael Lauria as they delve into the intricacies of post-intubation care and the critical factors that impact patient outcomes during the first 10 minutes after intubation. Building on the well-established concepts of airway management and resuscitation, the discussion introduces the new acronym PHACTORS, which stands for Positive Pressure, Hypoxia, Acidemia, Cardiac Output, Transfer, Ongoing Pharmacology, Resuscitation, and Suction. Eric and Dr. Lauria explore how these elements play a pivotal role in the success or failure of post-intubation management, emphasizing the importance of maintaining vigilance during this critical phase. With practical tips, evidence-based insights, and real-world examples, this episode is a must-listen for anyone involved in pre-hospital critical care.
KEY TAKEAWAYS:
KEY TAKEAWAYS:
- Prioritize Post-Intubation Monitoring: The first 10 minutes after intubation are critical. Continuously monitor for hypotension and hypoxia, even if the initial intubation appears successful.
- Transition to Ventilator Early: Whenever possible, transition intubated patients from BVM to a mechanical ventilator as soon as possible to ensure consistent and controlled ventilation, which reduces the risk of over- or under-ventilation.
- Use Head-Elevated Positioning: Intubate patients in a head-elevated position (30 degrees) whenever possible to maintain functional residual capacity and reduce the risk of derecruitment and hypoxia.
- Suction Regularly: Proactively suction the ET tube and oral cavity to maintain airway patency. This helps prevent complications like ventilator-associated pneumonia and ensures optimal oxygenation.
- Be Ready with Push-Dose Pressors: Have push-dose pressors ready during and after intubation, especially in trauma patients or those with borderline hemodynamics, to quickly address any sudden drops in blood pressure.
- Assess and Manage Acidosis Individually: Not all acidosis requires aggressive ventilation. Consider the patient's overall condition, and tailor your ventilation strategy based on the specific type and cause of acidosis.
- Regular Sedation and Analgesia Dosing: Avoid under-sedation, particularly with long-acting paralytics like rocuronium. Set regular intervals for administering sedation and analgesia to ensure patient comfort and avoid awareness of paralysis.
- Proactively Manage Cardiac Output: In patients with compromised cardiac function, focus on optimizing preload, afterload, and contractility. Use fluids, inotropes, and vasopressors as needed to maintain stable hemodynamics.
- Secure and Streamline Lines for Transport: Before transferring a patient, ensure all lines are secured and organized to prevent dislodgement or kinking during movement. Keep access points readily available for quick medication administration.
- Understand the Impact of Positive Pressure: Transitioning from spontaneous breathing to mechanical ventilation can significantly impact venous return and cardiac output. Be prepared to manage these changes, especially in hemodynamically unstable patients.
Show Notes...
- A human, even when paying attention can deliver injurious tidal volume breaths that may go in "easy" but are probably injuring the lungs (Dafilou B, Schwester D, Ruhl N, Marques-Baptista A. It's in the bag: tidal volumes in adult and pediatric bag valve masks. West J Emerg Med. 2020;21(3):722–2021.)
- Not only are the volumes too big, but we likely WAY over breath for patients and that can be really, really bad especially after cardiac arrest or in TBI (common reasons patients get intubated...right?) (Dumont TM, Visioni AJ, Rughani AI, Tranmer BI, Crookes B. prehospital ventilation in severe traumatic brain injury increases in-hospital mortality. J Neurotrauma. 2010;27(7):1233–41.)
- More issues with BVM ventilation that shows it's not consistent
- Siegler J, Kroll M, Wojcik S, Moy HP. Can EMS providers provide appropriate tidal volumes in a simulated adult-sized patient with a pediatric-sized bag-valve-mask? Prehosp Emerg Care. 2017;21(1):74–8.
- Turki M, Young MP, Wagers SS, Bates JH. Peak pressures during manual ventilation. Respir Care. 2005;50(3):340–4.
- Kroll M, Das J, Siegler J. Can altering grip technique and bag size optimize volume delivered with bag-valve-mask by emergency medical service providers? Prehosp Emerg Care. 2019;23(2):210–4.
- Mechanical ventilation provides more consistency and automation of a simple task with monitoring parameters (alarms) that can make it safe and effective for paramedics to actually put their brain energy to important clinical decisions and complete other tasks (Weiss SJ, Ernst AA, Jones R, Ong M, Filbrun T, Augustin C, Barnum M, Nick TG. Automatic transport ventilator versus bag valve in the EMS setting: a prospective, randomized trial. South Med J. 2005;98(10):970–6.)
- Starting mechanical ventilation and safe ventilator settings in the prehospital setting seems to make ED providers more likley to put in the right settings and continue appropriate lung protective ventilation...at least in ARDS (Stephens RJ, Siegler JE, Fuller BM. Mechanical ventilation in the prehospital and emergency department environment. Respir Care. 2019;64 (5):595–603.)
- Here's a really solid position paper from NAEMSP on it that kind of summarizes everything including the specific clinical times when it may be more helpful like cardiac arrest, trauma, etc (Baez, A. A., Qasim, Z., Wilcox, S., Weir, W. B., Loeffler, P., Golden, B. M., … Levy, M. (2022). Prehospital Mechanical Ventilation: An NAEMSP Position Statement and Resource Document. Prehospital Emergency Care, 26(sup1), 88–95. https://doi.org/10.1080/10903127.2021.1994676)