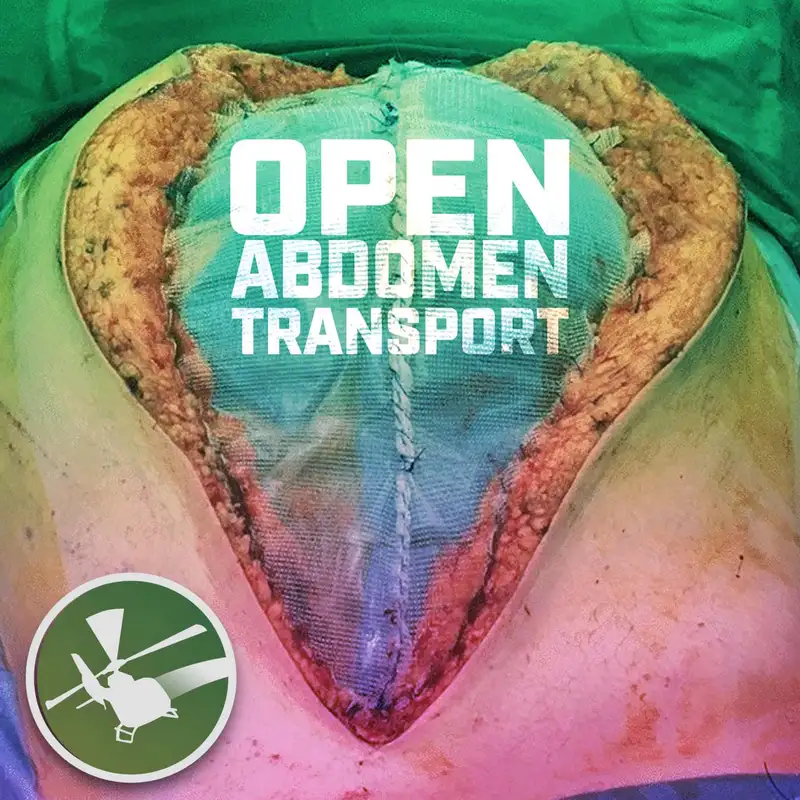
MDCAST: Open Abdomen Transport
Download MP3The content of this podcast is based on medical fact and evidence based practice from credible, authoritative sources, but is not a substitute for your institution's policies, procedures, common sense or good judgment. The views and opinions are those of Eric Bauer and flight bridge ed in their entirety. This is the flight bridge Ed podcast, critical care and emergency medicine education for nurses and paramedics.
Hello everyone, and welcome back to the flight bridge Ed, MD cast. My name is Mike Gloria. I'm an EMS and ICU physician with a special interest in critical care, transport and today, I am joined by another amazing guest, Dr Bryce Taylor, who actually has a pretty significant history as a flight physician. Worked in residency with a Carilion Clinic lifeguard and did fellowship, did a specific aeromedical fellowship at the illustrious University of Wisconsin in their med flight program, where he stays flying as a part time flight physician faculty there, and also has a very unique and broad spread in the emergency department, working in urban, suburban and some rural settings. And I'm super stoked, because Bryce and I are going to talk about a really cool topic today, which he actually brought up, and apparently at Carilion they did somewhat frequently, which is transporting patients with open abdomen, so a belly that is not closed. So this is a pretty unique and and cool population that we may see in critical care. Transport always got to love some surgical critical care. So Bryce, welcome back to the show, sir. Yeah, thanks for having me. Oh, pleasure, pleasure to have you back, my friend. And this is such a cool topic. I am so glad you brought this one up, dude. Well, let's just get get right into it. Let's start out with so when we say open abdomen, what are, what do we mean?
An open abdomen is pretty much a catch all umbrella term for a surgical critical care patient that left the or or left the procedure room with an open abdomen. Generally it is following an explorative laparotomy, where they actually do like a midline incision, basically from the xiphoid up to the pubic symphysis, they will often leave the patient open for several different reasons that we'll talk about.
Gotcha guys, when you get the page like, Hey, you're going to pick up a patient with an open abdomen, how do you approach it, like, in terms of and what questions do you ask in terms Okay, so what are some of the reasons why would a patient come out of the or and have their belly left open,
yeah. So I think, you know, definitely getting the good story about the what, the why, the how, the what procedure and the reason why they're still open is, you know, imperative. There are two, you know, really big critical care reasons why you might get an open abdomen. And then there is a third that is still critical care, but it's kind of a lower acuity critical care, I would say. So the two big, you know, big, mean, scary ones are going to be they did an emergency X lab to do damage control, resuscitative maneuvers and procedures and packing, and they are open still so that they can go back to the or once they get to their receiving facility. The other one is because of a condition that, as emergency physicians, we may miss up to 40% of the time, called abdominal compartment syndrome, which is basically a condition where the pressure inside of the abdomen increases to the point where it compresses all the vasculature, all the venous return, and leads to basically cardiovascular collapse, unless you decompress it. And so they will go in, they will do that midline incision. It's actually called a decompressive laparotomy, at that point. And then with that they are their end goal is to release the pressure, to temporize the patient, to get them to the point where they can survive transport to the tertiary center. The third is still it's more of an emergency general surgery concept. So you get patients that get pretty sick from like bowel obstructions or intra abdominal abscesses, flag bonds, stuff like that, and they will go in and do an initial source control or resection, and then they will leave the abdomen open and transfer to the tertiary center with plans to go back. But the abdominal compartment syndrome and the damage control resuscitation are the two big, really sick patient populations. And
I think one of the, one of the things we're going to harp on, and one of the things that I really wanted to impart to cruise is a lot of the time that it is. It's the open abdomen is like the frosting on the cake, but the real meat and potatoes the cake is what's going on with their damage control, or their abdominal compartment syndrome and all the other issues that it's caused, which is really why they require a lot of critical care support and why crews have to be. On point, the belly itself being open is like, really eye catching and intimidating sometimes, but managing some of the other stuff that came along with why they got the laparotomy, I think probably the most challenging, would you agree? Yeah,
having a good, well rounded critical care resuscitation while also managing the open abdomen component is definitely a challenge, especially if you're flying tin can 2000 feet in the air.
Agree? So as before we get into, like, a lot of the the physiology and the stuff around the damage control and the abdominal compartment syndrome, let's just like, try and draw a picture for everybody, like, what are these? What are these patients look like? What does their belly look like? What's going on in their belly when, like, they come out to the ICU and we're getting ready to transport them, when
you walk in the ICU room, they will, 99% of the time, look very critically ill. They should be intubated. They should be on a ventilator. They should have multiple drips running. When you look at their abdomen, is usually the first thing I do when I walk into these rooms, just because I'm kind of curious, but also like, I'm like, how, how difficult is this going to be? You'll see a few variations and how they will be packed up and, you know, ready for transport. A lot of this will depend on where in the hospital they actually had the procedure. So if they had the procedure done in the ED resuscitation room, it's going to look a little bit different than if it was in an ICU room or in an or basically, the big thing that surgeons are wanting is that they want sterile surgical towels that are soaked In sterile saline over the exposed area within the abdomen. Now, whether or not this is for an abdominal compartment syndrome versus a damage control resuscitation is going to kind of dictate what looks what it looks under those towels, but they want to kind of cover that to keep the bowel from getting dried out, but also to hopefully conserve some warmth. As far as what is covering these towels? If you are unlucky, it may just be the towels, in which case I would at least ask to see if there is something else that we can add on top of that, just because that is not very sterile, I think the likelihood of that happening is very low, especially coming out of a procedure like that, they are usually able to at least put an occlusive dressing over it. If it was a procedure done in an ICU room or an emergency department resuscitation room, they will probably, I would say, more than likely, have something called an IO band covering it, which is basically sterile, tough, sticky saran wrap. They actually will use it when you are prepping for a procedure. They will do the sterile technique, and then they'll put the IO band down, and then they'll do the incisions through that. But it also can work, because it can hold a fair amount of tension, but it also is an inclusive dressing, and it will go from the right to left side of the abdomen. It'll hold everything in, and it's pretty reliable. Now, if you have this patient coming from an or, or, they went to the OR, and then they came back to whatever room you're picking them up from. They will probably have an Evan Thera on, and that is basically like a, like a suction vacuum pack. It is a pretty cool device because it will allow for direct pair to nail resuscitation with closer control of the fluid in the cavity. It'll also allow you to keep suction on, and that is the most opportune mode of keeping the wound closed. I think an IO band is honestly gonna be usually enough, depending on on what you see. Yeah,
I kind of lumped them into two categories, like the basically dressings with or without vacuums on them, yeah, and the vacuum can be the answer is really nice. I agree with Bryce and that, at least in our institution, that's how they that's how they're coming out. I forget what the other brand names are for these dressings, but just like to put a picture in everybody's head, basically what it is. It looks like a large flap of plastic with little foam, either squares or long rectangles in it that allows for fluid to kind of percolate up through the abdomen and then getting drained out into the sterile foam and getting kind of suctioned into a central vacuum port. And that allows, as Bryce was talking about, the fluid control in the belly, alternatively and in some rural settings, or in some damage control settings, or if it was a bedside procedure you can do. I've seen small chest tubes. I've seen Blake drains. I've seen other things that actually get inserted into the towels that will come out and will act as vacuum dressings as well of one sort or another. So there's various ways to do it, but I just kind of think about them as there's drains and vacuums going in there and able to manage some of that fluid and drain some of that fluid off or not. And
my biggest thing is I just want something occlusive over this incision, yeah, and
I think that that's totally reasonable. And personally, I've never experienced that. I imagine it does happen some places. I've always. Seen them with either Evan or whatever dressing up. That's one thing I would say, cruise like, if there is no like vapor barrier, if there's no bio barrier over those towels or packing, I think it's totally reasonable to ask the sending physician, who's usually a surgeon, to just, to just put the eye of band over it, or put whatever, for so many reasons.
And in theory, Evan, like any sending provider, should be able to place an IO band. It's like
it's Medicaid. Is what I call surgical critical care arts and crafts, right? Like making different dressings and vacuum dressings and getting them to seal and whatnot is basically what it is. Okay, cool. So that's kind of what they're gonna look like. Those are the tubes and lines you might see. But let's get down to the meat and potato things, which is the two main reasons, the two big pathologies that someone would get an emergency procedure that requires lab, that requires emergency intervention in the admin, plus a lot of other organ system issues or critical illness, so damage control and emergency intervention for abdominal compartments. So start out with damage control. Let's talk about that. Bryce, these
patients can be victim to, really, any kind of trauma. Usually, in my experience, they've been far more blunt trauma than they have been penetrating. But penetrating trauma can definitely also, you know, play a big role, depending on what all structures are hit. I think the best way I can explain the setting that you're gonna get this in as a case that I had when I was a resident. We were in the Appalachian we were the receiving level one center. So we had a lot of little, even standalone, eds that would send to us. We had a an MVC with the driver, kind of Perry arrest the entire time through extrication. She coded on the way to the ED. They ended up getting Ross, but she had a super positive fast like, they just, like, put the probe, like, near her abdomen, and could see the free fluid. They were fortunate in that they had a surgeon. There it was, you know, daytime hours, you know, the surgeon was actually in the ED when they came in, and they actually opened her upright in the recess Bay. And their main thing with that was that in addition to doing the damage control, you know, product resuscitation and all of that, they also wanted to stop the bleeding. Now, when they go in to do this kind of procedure, their goal is not to fix permanently. Their goal is to temporize, to get them to the point where they can get, you know, they'll survive, transport to a center that can provide the, you know, the trauma, or they can provide the trauma, surgical, critical care needed, pre op, post op. So what they do is they do the X lap. They go in and they suction as much blood as they can. They try to visualize, like, you know, the culprit lesions that they can but I would say that half the time they are not able to visualize all of them. And then they go from each zone within the abdomen, and they pack it. In addition to this, they'll sometimes use, like, hemostatic foam. Sometimes they will do procedures where they kind of rotate the liver, but they do anything that they can to stop the bleeding. Once they have stopped the bleeding, they continue the blood product resuscitation, and then they do the abdominal dressing. So that's going to be either with the app there or the IO band. Now, since this one was done in the ED, she came with an IO band. Now this one is gonna look a little bit different than the abdominal compartment syndrome or the EGS patient, because they their abdominal cavity is gonna be packed full of, you know, surgical packing foam looking stuff. It's gonna look pretty messy. And this is all gonna be under the, you know, sterile towels that have been soaked. But you'll probably get some oozing around the dressing. She was Peri arrest until she got to the level one, actually, so they'll be, you know, critically ill beyond this, even if you get the bleeding stop, you're not done. You have to keep, you know, resuscitating, a full body balance resuscitation, and these ones are a little bit tricky, also because you're going to want to have them paralyzed and sedated, and that could be difficult with the tenuous blood pressures and everything like that. But basically the damage control resuscitation is they go in, they pack it, they achieve hemostasis as much as they can, and then they cover it, and then they try to get you to a place that has a level one or a level two, or
that was that was such, like a revolution for me, like a revelation for me, rather, when, like, because there's like, a paramedic, I'm like, Oh, they go in there, they got to be, like, looking for an artery and, like, ready to tie it off as surgeons. And when I realized, both in military and the civilian world, when they're just going through, like, super fast, and get into the abdomen, rotate the liver midline. Look back there, pack, pack, pack, rotate the liver laterally, then get underneath the liver. Look, look for any major bleeding, pack, pack, pack, and just really quickly going through the belly and essentially, like, super packing it. So they look like they have, like, a pregnant belly full of like. Hacking and gauze, and then the resuscitative phase of things being fixing the metabolics, getting their lactate down, etc, etc, etc, getting their blood pressure up, reversing their coagulopathy, being like, really the meat and potatoes. And this is one of the things that I think again, to hit on this and highlight it is why it's so important for critical care transport folks, because a lot folks, because a lot of this is bread and butter critical care, right? It
just looks scarier because the open abdomen in front of you, but every day we, you know, do product resuscitation, we give calcium, we correct the lactic acidosis, you know, we do the vent control. Yeah, exactly.
Now, let's transition away from the mostly the trauma side to the non trauma site. And let's talk about abdominal compartment syndrome, because you hit on something that was really, really important, that this can go underdiagnosed for or missed as a diagnosis for a while, and it can wreak havoc on a lot of the various organ systems and cause a lot of metabolic damage. It can be really sinister, but when it finally peaks and it's really bad, it can be bad and requires surgical intervention. So would you mind talking a little bit about what compartment abdominal compartment syndrome is, how we identify it, and all of the havoc and the various organs it can cause,
just like in all of our extremities, the abdominal cavity is actually a compartment, you know, lots of important things go through it, your IVC, your aorta, your kidneys, you also can have, you know, your diaphragm is not a solid piece of equipment. It will extend up into your chest cavity if pressure is applied to it. So abdominal compartment syndrome occurs when, for some reason, you get a massive increase in your abdominal pressure, and then that, in turn, will compress on the IVC. It'll compress on the aorta, it'll compress on the renal veins and arteries. It'll push up into the chest. It'll decrease your ability to oxygenate. It'll cause diastolic failure with compression in the media signum, basically you get abdominal compartment syndrome spiraling out of control, and then every single organ system will ultimately fail. So there's the World Society of abdominal compartment syndrome. They are a pretty cool society based off of like a surgical critical care global initiative to actually recognize when abdominal compartment syndrome is happening. There's estimates that emergency physicians can miss abdominal compartment syndrome up to 40% of the time, and then either it just is not recognized at the time of death, or by the time it's recognized, they are too far unstable to undergo anything procedural, like they'll die on induction. So it's a highly morbid, highly has a high mortality, and it can be potentially reversible if recognized. I kind of look at abdominal compartment syndrome from two lenses, so you got your primary causes. So anything that is a reason why you would have increased pressure inside of your abdomen. These can be like malignant ascites. It could be trauma, leading to, you know, lots of blood being in the compartment which gets open impact for hopefully, and that'll alleviate that. It could be from like perforation with a massive neoperitoneum. It can be from necrotizing pancreatitis, but it can also be secondary. So you get, you get a really bad trauma code, come flying in. They have been resuscitated in the field. They had, you know, all the regular code things done. They've had lots of fluids given to them during the resuscitation, lots of blood resuscitation, and then two hours later, in the sick, you all of a sudden, they start liking high peak pressures and dropping their blood pressure, and everything starts to fail. And then, you know, their abdomen is just standard, and that could be because they got ischemic bowel from having a global hypoxic insult, from being coated. They could have validema from either the hypoxic injury or from, you know, massive over resuscitation of the volume that generally is the undetected abdominal compartment syndrome. In either case, the management is alleviating that pressure before we get
into management. Can we just talk a little bit too? Because I think one of the challenges is a lot of the time the diagnosis is contingent on pressure, and knowing, I think those pressure both the clinical side of things like understanding the end organ damage, plus the pressure is important, but also how we manage that pressure. So when we talk to our we're managing we're measuring it accurately. And when we're talking to our colleagues, we're like, their abdominal compartment pressure is really like they know that we're like, we can explain how we're getting it and why. So could you just go through, like, those general like pressure ranges and like how we should be measuring that pressure Bryce,
the normal abdominal pressures are going to range between five to seven millimeters per mercury, and obese or pregnant. Patients, it can range up to 10, and within these ranges, they should not be affecting any organ system failure. Now, once you get an abdominal pressure up to 20, you are at a high risk of having multiple organ failure. I start getting concerned. Once I get a pressure of 17 or 18, not necessarily that I'm going to have anything actionable, but it's going to be something that I'm watching. Once I get to 20 then I'm, you know, even more concerned now you get this pressure, the gold standard is with a pressure sensing Foley catheter that measures bladder pressures. The thing with this is that you will hopefully have a Foley catheter in that can measure a pressure when you get to the patient, but you won't be able to measure it necessarily during the transport. So you want to be really sure that they are within our appropriate pressure for transport, and you want to be confident that they will stay that way, because if they spike their pressure up in the air, there is pretty much nothing that we can do other than try to chase our tails with resuscitating from above the head basically.
Yeah. So it can definitely be very challenging. I would add just a couple things. Bryce brought up that when the Foley is in, you can, you can measure that pressure. Technically, this is supposed to be done with them completely flat and paralyzed. That said. It's not always, you know, it's one thing, if they're, like, sitting up, or they're at an angle 20 to 30 degrees, which is good Venom ventilator management, usually. But just like, make sure that we understand that if they're mechanically ventilated, they're not 23 degrees, we should lay them flat to actually, like, measure the pressure. If they're really sedated and super calm and not doing anything. It's reasonable to say that pressure is probably, probably close to what it is. And if it's that they're laying flat, even they're not paralyzed, relax compliant with the ventilator and their abdominal compartment pressure is 62 like, you know, there's a problem, right? But technically they should be paralyzed, I would add that, and usually I don't do this, but it is possible, and in full transparency, like I don't, I wouldn't say we fly or transport these patients on like, a monthly basis. I've only known this, like a handful of times in the past few years. Is essentially you can use the pressure transducer for your normal a line, and that whole setup to actually measure the bladder pressure continually, essentially, like we do in the ICU. It's possible, I would say most of us don't do that, because that's like, that's like, quite a bit, and it's hard to interpret the changes as you're moving someone in and out of the aircraft and all this other stuff. And you got to re zero it, but you can do it. So if, like, the if their ICU, if the sending facility is like, I don't know what you're talking about. What you're talking about. You can hook up a pressure transducer from like, a normal a line, and get a pressure and get an idea. And usually, I think it's fair to say I would just spot check it. Like, like, everything, if everything's okay, good. If it's like, borderline may be reasonable to continue to measure it in flame, but I agree those are like, generally, good, like, pressure markers, pretty much the same ones that I use in terms of, like, getting kind of concerned. Let's talk about, like, some of the consequences, like when your abdominal compartment pressure goes up, and it's not because you're morbidly obese, and it's not because you're growing a baby in your belly, and it's very sudden, what kind of problems can they cause in the in your other organs, I
would say that the ones that really stick out for transport reasons are going to be up in the thorax, so your diaphragm will push up into your chest cavity. It'll make it so that you are not able to ventilate. You'll get high peak pressures. This will also decrease gas exchange. As there's going to be increased alveolar dead space, you're going to lead to hypoxia, hypercarbia, basically just pulmonary nightmare. Now, this alone would be enough to ruin my day, but this also leads to obstructive shock from the heart being compressed to the point where it's not actually able to fill with each heart beat. You end up going into shock, that's going to be refractory to any kind of intervention that you do, up in the air. That's not to say that these are the only or the most important. I think that all of the consequences together are going to be what's important. But you'll get kidney failure because your abdominal vasculature is going to be depressed. You're going to have decreased renal perfusion, it'll lead to atn, and then your kidneys will just go ischemic. You'll have the later stages where it'll activate the sympathetic nervous system. And then, basically, one of the hallmark signs of abdominal compartment syndrome is that you have a decrease in your urine output, and then you have a complete stop in urine output. So this is something that you can monitor pretty easily while in flight, because they should have the Foley catheter in with the GI system, you have splanchnic organs that are going to become hypoperfused and then ischemic. That'll lead to basically just diffuse gut death. This will worsen the abdominal pressure. It worsens the risk of bacteria. Translocation. But also, if you get a patient that has an entire length of dead bowel, you know that can be not salvageable when they go in to try to resect it, you know that can be a death sentence. Now, when you look at the liver, you'll get decreased perfusion to the liver, because the abdominal pressure is pushing up on it, pushing on all the vessels and veins and everything that's bringing stuff in and bringing stuff out. With this, you'll be unable to clear lactate, so you'll get a crazy lactic acidosis, which will lead to just a highly deranged acid base status that'll make resuscitating a complete nightmare as well. One thing I found kind of interesting was that your ICPs, your intracranial pressures, are actually affected by your abdominal pressures, so your ICP and cerebral perfusion will decrease, especially with CVP decreases, so you can actually suffer neurological, hypoxic injury from having abdominal compartment syndrome that can lead to lasting deficits if the patient is to survive.
I love the way you phrase that. I think the most apparent things to us are the hemodynamics and oxygenation and ventilation. Those are things that are going to start beeping. Things are going to be on your monitor that you're going to see, and you'd like, oh crap, when you fix those, but it just wreaks havoc. Like all these compartments in the body. When you have huge, super high pressures in the brain, it causes problem in other organs remotely. And then when you have really high pressures in the belly, he does very, very similar things, getting shock liver and acute kidney injuries and all these other things. It's pretty wild. Really, really. I mean, it's cool from a path of physiological standpoint, it is awful from from a patient management standpoint. So much to do cool. So those are excellent, excellent points, good stuff to look for. So think about guys elevated intra abdominal pressures on clinical exam that are causing other end organ problems. And those problems can be hemodynamics. They can be problems with oxygenation, ventilation, and specifically high or issues with compliance, pulmonary compliance, high plateau pressures and P pressures in the ventilator as well as acute kidney injury with ulurgia, so low urine output. And you know what? All the other problems that Bryce talked about, pressures plus end organ damage equals abdominal the diagnosis of abdominal compartment syndrome. So let's get into now, before we get into overall like management of these patients with open bellies. Let's focus on the abdominal compartment syndrome patients for a second, and let's just say that they don't have an open belly yet, because this is a super important patient population that we can help with potentially, and you're taking them from a rural or smaller, critical access hospital to a surgeon for intervention. What can we do for managing these ACS patients? I would
take a look at this situation. I would look at how ill this person is. You know, a lot of this is Gestalt. You know, numbers are good, but you want to treat the patient, not the numbers. Ideally, if they are a true abdominal compartment syndrome, you want to have them get the decompressive lap rotomy Before you even start spinning your rotors, because the likelihood of a quick death in these patients is very high, especially if you get cascade of inflammatory markers going off, lots of ischemia just catching up to you while you're in the air. Depending on how long your transports are, there's gonna be nothing you can do about it if they code up in the air. I know that not all centers are capable of this. Not all centers have a surgeon, not all centers have an ED physician that's willing to do a decompressive laparotomy. I would say that most are not the best way you can go about transporting these because your next best step is going to be getting them somewhere that they can get the decompressive laparotomy, which is going to be your destination is you're going to want to do everything you can to decrease the amount of pressure that is applied to the abdomen and decrease any kind of pressure that could be applied from the abdomen. So you want them intubated. You want them supine, length, completely flat. If you have a critically ill patient and they are well sedated, sometimes you just have to paralyze. To take one thing out of the equation, if they are well sedated, and a lot of times this can be chasing your propofol with Levi fed, or keeping the Neo stick and a NEO drip going, just get them well sedated. And sometimes paralyzing them can just decrease all the pressure, because it decreases the muscle tone, that'll also make them more compliant with the ventilator as well, which can help because if they're bucking the ventilator, they're increasing their abdominal pressure, they're increasing their intrathoracic pressure, secondary to that, decreasing their venous return. The other thing is that you want to be really facile with the ventilator. Anything you can do to keep the intrathoracic pressure down is going to help you so small tidal volumes with a fast rate and then lower peep are the moves that I would make to transporting these patients. Everybody has end tidal CO two now, which I think is wonderful. I use it in the ED all the time now too, not just in the helicopter. And don't be afraid to go fast with your rate, as long as you're getting equal to. Metal volumes in and out, you're doing okay. You also really want to avoid over resuscitation. If you can't, if they're on pressors, see if you can double concentrate the presser as they drop their pressures, you're going to want to quick reflex to dumping fluids in them, and this is going to ultimately not be helpful once they do get the decompressive laparotomy, because this fluid is going to go straight to being gut edema. And that kind of is a rock and hard place. I know it has level three data that was released that said, resuscitate robustly, but avoid over resuscitation. And they define over resuscitation as being 10 units of packed reds or greater, or more than 15 liters of crystalloid, you know, it's level three evidence, so not great. However, you know, stuff like this is hard to research on, but they kind of stand behind the the idea that 15 liters of crystalloid is going to increase your likelihood of ACS. So see how much they got before you got there, and then try to limit what you have during transport. And
we'll talk a little bit more about the over resuscitation here shortly. But I just wanted to piggyback on a couple things that Bryce said. Like I said, we'll talk about the over resuscitation here in a second, because I really want to foot stop that, but the paralysis again, like as Bryce indicated, I think as long as, as long as you have really good sedation, there's not strong evidence for in this patient population, but there's also, if they're intubated, mechanically ventilated and well sedated, probably not a lot of downside to short term paralysis for these patients, especially as a bridge to getting their belly open and treating their abdominal compartment syndrome. And same thing with the ventilator stuff. I know we've had some discussions on this podcast about the dangers of elevated mechanical power and really fast or mechanical ventilatory power and really fast rates. That's really in the setting of ARDS, again, as like a temporizing measure to maintain their minute ventilation so you can get them to definitive care. Probably, I would say, without really robust evidence, that the benefit probably lays in ventilating them and oxygenating them adequately, even if you have to at least temporarily use pretty high rates. The last thing, and this is highly controversial, but I did want to bring it up, and I will always say, defer to your local guidelines and protocols. But something to think about. Something to think about is that if their abdominal compartment pressure is elevated, and you really want to maintain kind of like the brain right, a compartment pressure, perfusion pressure of that compartment, whether it be cerebral perfusion pressure or abdominal perfusion pressure of at least 5055, 60. Again, there's a lot of disagreement on this exactly what it is, and we don't have good data to say what we should be shooting for. That said, if you know that they they are not getting a decompressive laparotomy at that critical access facility, and their abdominal compartment pressures are high, it may be reasonable to run their pressures and keep their map instead of running at 6065 if you know they're intra abdominal pressures are in the 30s or higher, potentially pushing that mean arterial pressure up into the 70s or even the 80s, to make sure their gut is perfused again, as a bridge to definitive intervention. No real strong evidence for that, especially in the transport setting, but it's something I would discuss with the sending and receiving physician, if they think it's appropriate. I would argue that perfusing your kidneys and your liver and your gut for the next hour or so, even if it requires a little bit of pressures, is probably a reasonable way to go. Would you agree? Bryce, yeah, I agree. Now let's, before we get into again, a lot of the transport management details, let's touch on that, that third, that sort of third group, those patients that go not necessarily because they have elevated abdominal compartment pressures, they've been shot in the belly, but let's say they have an obstruction, or, like, a perforated viscous or, you know, an exploding pancreas, or something like that. They get to get some other emergency, general surgical intervention. So let's talk about that patient group for one second. So in
surgical specialty hospitals, anytime you go in the sick you there's gonna be probably three or four of these on the unit. They are not uncommon. They, in the moment, feel like they might be less sick than the compartment syndrome or the DCR, but they have a lot of potential to become very sick. You know, they're not something to really get lax about. So open abdomens from an EGS case, basically any kind of procedure that's done to correct something that occurred within the abdomen that's not from high pressures and not from a blunt trauma or gunshot wound. So, you know, you could have the small bowel that was causing gut ischemia that had to be resected emergently, or you could have a perforation that led to, you know, just lots of it's called a. Speculant material called succus, being just expressed all throughout the abdominal cavity. Basically, they open up and they either want to fix what's ischemic or they want to source control. So the source control addressing the ischemia are important, because if they're not addressed, they will lead to septic shock that could become refractory and when it's time to go to the or good luck with induction, because they are going to be circling the drain. So they will go while the patient is stable, and they will do their source control or their resection. And then after that, they will leave the patient open, because there's going to be an anticipated go back to the or to either just reevaluate. A lot of times they just go in and they look at the post op area and make sure that everything's an app like the anastomoses, are all intact. Or, you know, they just want to make sure there's nothing, nothing else that they have to really control in there as far as source goes. And then sometimes it's just so that they can go back and they can do a re anastomosis, where they actually recon connect anything that's resected. Or usually it's within 12 hours of the initial procedure. So they come back to the ICU, they're open, they usually look pretty good. What is scary about these patients is that anytime a knife is taken to a patient, they are going to have an inflammatory response. With these post op patients, they will come back looking okay for about two hours, and then they're going to have a massive cytokine release. They're also going to have a mobilization of any of the pathogens that might have been, you know, seeded from the source control, or seeded from before they went in. You know, they is, they have a very high likelihood of having an acute decompensation, probably, you know, if you're lucky, while in the air. Basically, you just get a flash septic shock that you have to be anticipating, and you want to be watching closely for so that you don't fall behind and end up, you know, chasing your tail with resuscitating. That's
another really important point about these patients. They'll go from the ED, or they'll come from the ICU, and they're awake and in maybe a lot of pain, and you identify the primary pathology, they get intubated in the or they get their belly open and they come out on two or three pressors. And because of that and cytokine release and that massive systemic inflammatory response, and often, I think, if it's as small critical access hospital or a hospital without a larger tertiary ICU to manage a lot of the complications and whatnot, and they're getting shipped somewhere, we are going to see that they're going to be coming out of the or they're going to be calling us for transport when they're in the or shortly after they get out of the or, and they're sitting in a small pack, you someplace, unlike three pressors and and that I think we have to be, that we have to be prepared for. And I know a lot of you who are ICU nurses out there have seen this, right? You have, like, a patient that's actually doing okay. You've weaned down their presser, they're going back to the or they get their belly reopened again, and they come back, and now they're on a lot of pressor and then that presser requirement will decrease over the next 12 to 24 hours. So anytime this happens, they get that pretty substantial cytokine response. I think we should be prepared for that. So if you, if you get a call that they're in the OR, and on like a little bit of pressure, they're going to the OR, and then you transport and they're going to come out of the or, be prepared that they will likely need more hemodynamic support. The other thing I think Bryce touched on, that I really want to impart to our listeners is knowing the plumbing. And I kind of put this into three groups in my in my head, right? The plumbing is normal. So they've done primary, re anastomos and hook things up, and everything is draining out the bum like it should. They have diverted plumbing so they have an ileostomy or colostomy, so they still have something tied off distally, but we are able to drain stuff, and they are in discontinuity, so everything is tied off. So these patients, and I would say especially for emergency procedures and damage control procedures, this is not uncommon that both things will be tied off, so both proximally and distally, the bowel will be tied off, which means nothing by mouth, no, no stuff should be going the OG tube or anything like that. So know the plumbing too. All right, yeah, always know the plumbing, whether it's your house, your RV or your patient, know the plumbing, all right, so let's talk about managing them during transport. So we kind of went through why patients get get these interventions, why they come out with their belly open? And we hit on the two big things, which were down or two, plus, like a minor thing, damage control, abdominal compartment syndrome, and then all so the other EGS grab bag of reasons why they would come out with an open belly. And now managing this patient transport. So let's go through Bryce some of the key aspects of managing these patients in flight.
You know, as with every single one of our patients having an overall aggressive general approach to critical care is important. They are a critical patient with an open abdomen. They're not just an open abdomen. So you want to know the hemodynamic parameters at the. Surgeons want that are most optimum from their you know, their condition, and you want to do everything you can to keep those parameters in check. One of my coworkers likes to say it should be eventful on the ground and flight should be uneventful. And I think that this is really one of those cases where that really stands true, because if you can resuscitate, do the critical care needed on the ground, get them in a good place, and then just take a ride to the receiving center. Yeah, that's great. Then deliver your open abdomen, and then it was a good flight. But you need to be able to understand and really recognize any kind of subtle changes in those hemodynamic parameters, you are going to want to be really judicious with the fluid resuscitation, but you also want to know why they are in shock. Are they distributive because they're getting a cytokine storm from their recent procedure? Or are they losing blood into their abdomen again, or are they building their abdominal compartment pressure again? Being able to recognize that can help you lead you to the correct resuscitation manner. Somebody who's developing an abdominal compartment increase in pressure that's leading to them having an obstructive shock. If you flood them with another 10 liters of fluid, that's not going to be good down the road. However, if you know, you get somebody that was a DCR that is starting to bleed again, you know, there's a lot of output from their drains. Knows, blood from their you know, their dressing, soaking through their towels and stuff like that, then, yeah, you probably do want to administrate blood products. So I like to double concentrate my pressors. If not hemorrhaging, I would be very cautious with the fluid administration.
And I think there's two things that I think you said there Bryce, that are super important. One, if you're going up on your pressure or having issues with hemodynamics, do not assume that it is just because of their septic or they're having an inflammatory response. They can bleed. They can have other problems. They can have other new they can have pneumothoraces. They can have all sorts of other stuff going on. So don't just throw fluid impressors at them, assuming it's their belly. Really have a good think about like, is it something else that's contributing? Generally speaking, that's probably the case. It is the belly. It is the inflammatory response, but the fluid thing, and this is me putting on my ICU hat. It is not benign. Consider fluid as a drug. It is not benign. I know it's easy. People say, well, they can take care of it in the hospital. They can take care of the ICU. They can diaries them in the ICU, not so much. It's not as easy as it sounds. Often they have acute kidney injuries, getting fluid off them turns into a big issue, and for this patient population in particular, this is loud and clear. For the people in the back, it can cause significant harm if we can't close these patients, right, if they have to close by secondary intention. Or less and less, I'm seeing prosthetics put in, so meshes and that sort of stuff to help close the admin those patients are at substantially high risk for infections, fistulas, all sorts of very morbid long term complications. So a super edematous fluid, overloaded patient that moves all that into their belly, and we can't close their belly. Is a big problem that we can avoid in the transport in ED settings, resuscitative setting, in the transport setting,
one of my longest sick you patients was actually one of those failed prosthetic grafts, and it was an abdominal compartment syndrome case that led to it.
They can be really, really bad, yeah. But aside from the fluid resuscitation, the blood products, right? We kind of talked about analgesia, sedation and paralysis. We talked about the suction dressings, right? So a lot of these patients will come with suction dressings. And so the general guideline, this is Ed ICU, pacu, or transports the same, keeping it around like 120 to 125 millimeters of mercury, I think is, is a pretty reasonable setting. I would, for a lot of these patients, hook them up to suction a lot of time with with various tubes and lines. Like leaving them off suction for a while is not necessarily a huge issue for these patients. I would say it's part of the decompression. It's part of taking the fluid off their belly. It's part of optimizing organ perfusion, so make sure they're actually hooked up to suction.
I can also in the DCR patients. So yeah, tamponade, the
other thing I would relay to people is, before you get going, and Bryce touched on this earlier on is take a look at the dressing. Take a look at the dressing. What's underneath it? If they have an Evan Thera, or they have towels with a sterile biofilm or Evan over it, and other forms of drains, make sure it's actually draining. Make sure the drains are working as they're supposed to. And make sure there's just not a lot of blood leaking, or fluid leaking from around those drains. Generally, in the ICU, of like, you know, 2030, to 50, high end being 6070, 80, of serous Angus, or clear fluid coming out. Man, I'm not worried if it's pouring out blood or continually suctioning out blood, like on, you know, 5080, 100 cc's an hour, or it's like, leaky, like, you can't see the towels or the dressing because there's just blood underneath it, and it's coming out the sides the dressing. I would get the sending providers attention, and make sure you do that. Make sure you have a discussion about, like, is this a big problem that needs to be fixed here at the bedside or in the or, or are they okay for transport? In your opinion? Getting down to those two subsets, let's talk about let's kind of fast forward a little bit to those two subsets, damage control, resuscitated patients and the abdominal compartment syndrome patients with an open belly in flight. What else for the damage control patients? Do we want to pay attention to Bryce? I actually
think that this is probably important for both of them for different reasons, but for the damage control one, especially, you know, with any kind of hemorrhagic shock, you're gonna get a lethal triad. So if their abdomen is open, they are at a very high predisposition to dropping their body temperature. You know, you want to keep them warm. A lot of places have like the heat packs. I steal a lot of heat packs from the EDS, and, you know, just shove them all over the patient. Now, with the damage control ones, you also want to manage their acidosis. So that's going to be, you know, ventilatory compensation. I'm not huge on bicarb, but like, if they're Peri arrests, then you know, you can push it. They may have a bicarb drip going. Also, I've seen that a few times. And if they want that going, then, you know, like, whatever, and they replace the blood products with a balanced resuscitation. I hope that every helicopter has whole blood at some point, but that's probably not going to be the case for a while. And as far as, like, the sequence for blood product resuscitation goes, that's going to kind of depend on what they've gotten so far. If they got, you know, rotems or the thrombo elastograms, this can kind of help guide resuscitation, but most community centers don't have that. And then, if nothing else, then just do your normal plasma, red plasma, red until you get to your your center. The only other
thing I would add there is if you have to, and kind of Bryce touched on this earlier, if you have to go up on their minute ventilation help them compensate for a metabolic acidosis while they're clearing everything and they're washing out their lactate, or metabolize no lactate, their kidneys are kicking back in now. They got perfusion their kidneys also very reasonable and keep an eye on their urine output, regardless of what reason they got their open belly for their urine output is a relatively good indicator of perfusion to their kidneys and sudden changes, especially sudden drops, should spike your attention and at least prompt you to tell the sending facility, hey, like they were doing fine, documented, like 30 to 50 CC now are at the sending facility, and then all of a sudden, like this last hour, it's like zero for the past hour or two. Yeah. So they can at least have situational awareness and keep an eye on it, I would say. So let's talk about the abdominal compartment syndrome patients now. So you rescued this abdominal compartment syndrome patient that got decompressed. You're taking them in the in the aircraft. Any other pearls, things you'd want to pay attention to, Bryce,
they will probably still be unstable when you get them. I don't think I've ever seen anyone with abdominal compartment syndrome immediately post decompressive laparotomy. That has been any sense of the word is stable, but sometimes they're like stable enough to work with. The big thing you want to do with the compartment syndrome patients is you want to make sure that they don't still have it or it doesn't recur just because they there's kind of like when you break you get an open fracture of your arm, people seem to think like that means you can't get a compartment syndrome there because there's already a hole. You still can. And then that also applies to the abdominal compartment syndrome. Just because they got a decompressive laparotomy does not mean that they cannot have a recurrence. It can recur in up to about six to 14 patients. The way you're going to really detect it up in the air or during transport is you really want to be monitoring the urine output. So a sudden drop or stop in urine output is going to be kind of a telltale sign. Other than that, it's going to be kind of a clinical recognition so worsening acidosis, you know, worsening hypotension, high peak pressures, cardiovascular collapse, if you have, you know, like PSE labs, there might be, you know, elevating lactate with abdominal compartment syndrome. I really rely on the clinical signs and symptoms more so than really even the numbers, because when it's happening, it's there, it's apparent. Now what to do if you do get a recurrent abdominal compartment syndrome? If you get if you recognize it before you leave, you might want to talk to whoever did the decompressive laparotomy and see if they can go back in and either completely decompress it or figure out what's not decompressed or re decompress it. Now, if you're in the air, it's going. Be kind of more difficult. It's gonna be more of like what we talked about earlier. You know, your mom laying supine, good sedation, potentially paralyzed, and then optimizing the ventilator, and then trying to support the human dynamics as much as possible. Yeah,
and I forget if we talked about it earlier, but that that would include, in my opinion, things like decompressing their stomach and and whatnot, and trying to get any additional liquid or gas that's in the belly out of the belly, keeping them to suction, etc, etc, yeah, and that's a really good point, and one that I have heard, and we talked about this before the podcast a little bit, people say, Well, you know, like, yeah, their pressures were going up, and all this bad stuff was happening, and the pressures in their belly were in the 30s or 40s. But I didn't believe it, or, you know, they can't get environmental compartment syndrome because their belly is open. That is not true. That is definitely something that you should do all the non, all the non surgical things that we talked about for a patient that doesn't have an open belly, to try and optimize their abdominal compartment pressures, and then making sure the sending facility is aware. To the point where I've encouraged criminals, if you think it's really bad and like, there's no fix at the sending facility, or the surgeon has disappeared from the sending facility, and they need to get going because they're critically ill. Fine, but you know, give I would call ahead of time to receiving ICU vision, like, this is what's going on, so they can at least have a heads up. And if they're in the surgical ICU, if it's a surgeon, they're gonna know what to do if they're not. And if it's a, you know, mixed ICU, they can be like, Oh crap. Like, I should probably like, let the surgeon know, like, right now, so that when this patient lands, they can come to the bedside, we can have a discussion about how we're going to manage this. Because this is, this is not a this is not something that we can abide and just like let happen. So really, really good points there.
A lot of times they're going straight to the or too. I've noticed that that's actually
a really good point. Is that sometimes they will go straight to the or there are a lot of more and more facilities, depending upon how aggressive their surgeons are, will have direct to or transport protocols and capabilities, which I think is great, just get them to where they need to be awesome. So we basically, we went through and we talked about, so what do we mean by open admin, how they're going to come out, all the parts, pieces, tubes, lines, what it's going to look like, what to look for, and some of the main pathological processes that are driving this and or cause them to go and get a laparotomy and come out with an open belly. We talked about sort of the transport management stuff, any other pearls or tips or tricks you want to leave the audience with Bryce, it's going to
be stressful. Since you have a receiving that means that you have support in that receiving, they're aware that you're there picking them up. You can always call them. It's a common physiology. So any kind of center with acute care surgery is going to be well prepared to give you advice on how to transport with this. So I think just reaching out to your resources, in addition to having this all in the back of your mind is going to be be for the best,
exactly. I would say, lean on those resources, medical direction, receiving physician acute care, surgery and your trauma physicians, make sure we're doing really good, and all the supportive critical care, optimizing the perfusion pressure in their belly, making sure their mechanic so they're mechanically ventilated, which almost all of them are going to be, making sure their oxygenation and ventilation is appropriate, and keeping track of those plateau pressures it might be indications of rising intra abdominal pressures. Making sure they're hooked up to suction. We're draining their stomach. We have their up there hooked up to suction, and we're watching their urine output really, really well, and then taking care of all the other metabolic stuff that's going on. If they haven't, they generally will have had at least a dose in antibiotics. Make sure they're staying on their antibiotic schedule as well. So I would say that's transporting the patient with the open abdomen. Thank you everyone for tuning in and listening. Take care. Fly safe.
This has been a production of the flight bridge Ed podcast, leading the way in pre hospital critical care and emergency medicine education you.
Creators and Guests